If you experience any symptoms characteristic of low cortisol levels — such as abdominal pain, chronic fatigue, depression, irritability, or muscle weakness — you may have been diagnosed (or you may have diagnosed yourself) as having adrenal fatigue, HPA axis dysfunction, or some other adrenal disorder.
In this post, we present and describe a variety of health conditions related to the adrenal gland, some of which may be caused by dysfunction upstream of the adrenal.
With a greater understanding of the adrenal gland and dysfunctions that impact the adrenal, our hope is that anyone with symptoms of an adrenal disorder seeks out a professional medical diagnosis, like those offered here at BioDesign Wellness — the Tampa Functional Medicine practice — to find out what is really going on rather than try to self-medicate with adrenal support supplements.
Adrenal fatigue
In 1998, chiropractor James Wilson coined the term “adrenal fatigue.” He used it to describe a condition in which the adrenal glands, overstimulated by chronic stress, burn out and shut down, causing a variety of symptoms, including the following:
Since then, many books have been published, and many supplements have been developed to support the adrenal gland. Unfortunately, some people who follow the advice in these books or take these supplements have no idea what is really going on in their bodies.
As a result, the root cause of their symptoms remains untreated, and they may even be doing more harm than good. (For more information on Adrenal Fatigue, read our September 2018 post Feeling Burned Out? You May Be Suffering from Adrenal Fatigue.)
Adrenal disorders
Conventional medicine denies the existence of adrenal fatigue but recognizes several adrenal disorders, including these:
- Adrenal cancer is characterized by abdominal pain, weight loss, or overproduction of certain hormones, such as cortisol and androgens, which can also cause high blood pressure and high blood glucose, and (in women) increased hair and irregular periods.
- An adrenal incidentaloma is caused by masses or tumors larger than one centimeter on the adrenal gland, which may cause the overproduction of hormones.
- Adrenal insufficiency (Addison’s disease) is a condition in which the adrenal glands do not produce sufficient amounts of certain hormones, which can cause many of the symptoms commonly attributed to adrenal fatigue. Adrenal insufficiency is commonly broken down into two classes:
- Primary: Caused by damage to the adrenal gland as a result of an autoimmune condition in which the immune system attacks the adrenal glands, tuberculosis or other infections, cancer, or internal bleeding into the adrenal glands.
- Secondary: Due to the pituitary gland not producing enough adrenocorticotropic hormone (ACTH) to stimulate hormone production in the adrenal gland.
- Cushing’s disease: A condition in which the adrenal glands produce too much cortisol, which can result in weight gain and fat distribution mostly in the abdominal region, easy bruising, poor wound healing, thinning of the skin, round face, weak bones, fatigue, high blood pressure, high blood sugar, muscle weakness, irritability, anxiety, depression, mood swings, acne, increased thirst and urination, and (in women) irregular periods, and growth of facial hair.
- Pheochromocytoma: Tumors inside the adrenal gland, which can cause overproduction of epinephrine and norepinephrine, typically resulting in high blood pressure.
- Conn’s syndrome (primary hyperaldosteronism): Overproduction of aldosterone by the adrenal glands, which may result in high blood pressure, headaches, excessive thirst and urination, and muscle weakness or cramps.
HPA axis dysfunction
A relatively new diagnosis is being used in place of “adrenal fatigue” and “adrenal insufficiency” — hypothalamus, pituitary, adrenal (HPA) axis dysfunction.
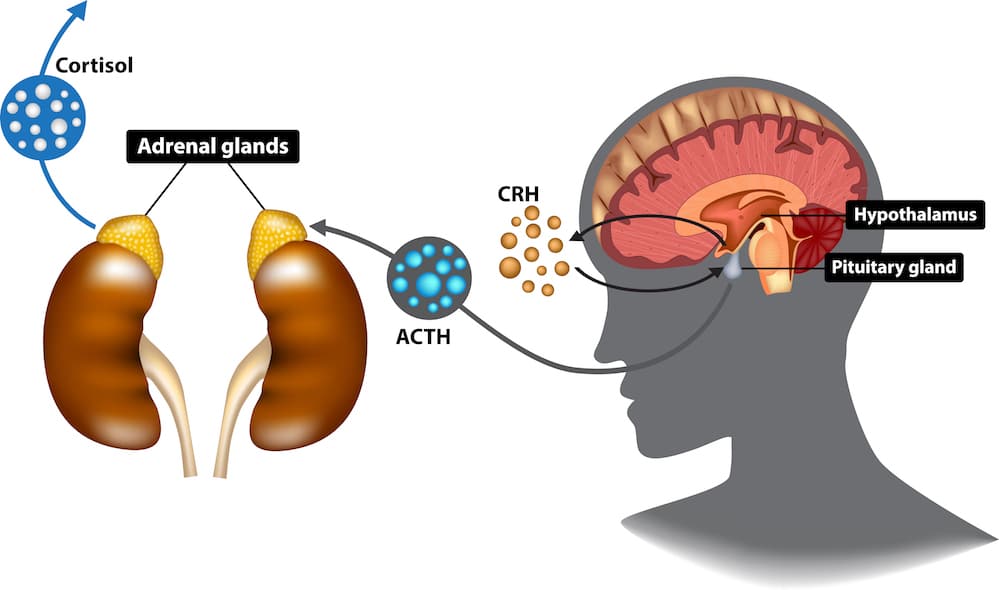
This diagnosis is more accurate than that of adrenal fatigue and adrenal insufficiency because it recognizes that the adrenal gland may not be producing sufficient hormones due to something upstream from the adrenal gland. “HPA” refers to the three components involved in adrenal hormone production:
- Hypothalamus: The region of the brain that enables the body to maintain homeostasis (equilibrium) by regulating sleep, emotions, body temperature, hunger, thirst, and so on.
- Pituitary gland: A pea-sized gland at the base of the brain that regulates other endocrine glands, including the adrenal.
- Adrenal glands: Small glands, one atop each kidney, that produce certain key hormones, including cortisol, aldosterone, DHEA, androgenic steroids, epinephrine (adrenaline), and norepinephrine (noradrenaline).
Working together, these three components regulate your energy levels, stress response, metabolism, mood, motivation, and immune system. Here’s how it works:
- In response to stress, the hypothalamus secretes corticotropin-releasing hormone (CRH) to signal the pituitary gland.
- In response to CRH, the pituitary releases ACTH to signal the adrenal glands.
- In response to the ACTH, the adrenal gland secretes glucocorticoids, including cortisol.
HPA axis dysfunction results when one or more of the three components of the HPA axis is not doing what it should be doing. For example, if the hypothalamus fails to signal the pituitary gland to release ACTH, then the adrenal gland won’t produce sufficient amounts of cortisol. The problem, then, is not with the adrenal gland but with the hypothalamus.
What is really going on?
People who suffer from HPA axis dysfunction are often undiagnosed or misdiagnosed and end up “chasing symptoms.”
For example, they may be taking antacids to treat indigestion or getting steroid shots to reduce inflammation caused by low cortisol. The root cause of their symptoms is never addressed, and the treatments they are receiving often do more harm than good.
Usually, the root cause of HPA axis dysfunction is inflammation due to a variety of stressors, including emotional stress (at home or work), undiagnosed infections, exposure to environmental toxins (such as toxic mold) and pollutants, and food sensitivities or poor diet.
Inflammation will cause dysregulation of the signals in the brain coming from the hypothalamus, causing a chain reaction that impacts the pituitary gland and, ultimately, the adrenal glands. This will have a “whole body” effect with a host of unexplainable health concerns.
Effective treatment typically involves identifying and reducing the impact of stressors, treating any underlying infections, reducing exposure to environmental toxins, detoxing the body, and adjusting the diet to eliminate any problem foods. Restoring health to the gut may also be necessary.
However, the first step is to obtain an accurate diagnosis from a doctor who understands the HPA axis dysfunction. If you or a loved one is experiencing any of the symptoms described in this post, we strongly recommend that you schedule an appointment for an examination and testing.
With an accurate diagnosis in hand, you can begin to treat the root cause(s) of whatever is ailing you and get back on the path to health and happiness.
– – – – – – – – – – – –
Disclaimer: The information in this blog post about HPA Axis Dysfunction and Adrenal Fatigue is provided for general informational purposes only and may not reflect current medical thinking or practices. No information contained in this post should be construed as medical advice from the medical staff at BioDesign Wellness Center, Inc., nor is this post intended to be a substitute for medical counsel on any subject matter. No reader of this post should act or refrain from acting on the basis of any information included in, or accessible through, this post without seeking the appropriate medical advice on the particular facts and circumstances at issue from a licensed medical professional in the recipient’s state, country or other appropriate licensing jurisdiction.